GID.info |
||||||||
| Gender
Identity Disorder Information |
||||||||
SURGERY for Intersexed People Sex Assignment Surgery on Intersexed People Sex Assignment Surgery is often performed on people who are intersexed. These surgeries may be performed shortly after birth, sometimes by doctors who do not tell the parents or gain their permission, or may be performed during adolescence or even later in life. It is not uncommon for intersexed people to undergo a series of surgeries throughout their lives. What is rather insidious about Sex Assignment Surgery is that, for the most part, such surgeries are medically unneccesary. Furthermore, that doctors have performed such operations on children without parental consent or knowledge, and often continue to lie to intersexed patients into adulthood. Many intersexed people consider such surgery equal to "mutilation" of helpless children, and the Intersex Society of North America is one organization fighting to change current medical practices that advocate such surgery on intersexed babies and children. The sex assigned to a newborn baby is often only based upon the appearance of its external genitalia. If they appear to be "normally" male or female then an baby that is actually intersexed may be unhesitatingly so assigned, and its real condition only discovered weeks, months or even many years later, e.g. at puberty. Only if there are ambiguities in the genitalia is further investigation likely before a babies sex is assigned. When deciding the "best sex" to assign to an intersexed child, the physician considers the following:
Such sex assignment is usually done within a few days of birth. However, occasionally a baby may be assigned to one sex at birth, but for various reasons the physicians later recommend its re-assignment to the other sex because of the discovery of viable testes in a supposed baby girl. The medical community's belief is that the earlier this re-assignment is done the better. It is relatively rare after about 24 months of age for such reassignments to be done, as many doctors believe that the baby's gender will be irreversibly set by then. Most of the doctors who believe this are still following the now outdated, and unfounded research of Dr. John Money (formerly of Johns Hopkins), who theorized that one could surgically assign a boy child as a girl, raise the child as a girl, and the child would happily BE a girl. In generaly the theory that a baby's gender is irreversibly set by 24 months may not be untrue - but there is no way of knowing, in an infant so young, what the true gender identity of the child IS. At best, the doctors get it right 50% of the time. The term "sex re-assignment" is also often used to refer to the deliberate legal and social sex assignment of a baby contrary to its chromosomal sex (e.g. assigning a "XY" baby as female), even if it was never actually assigned to its chromosomal sex.
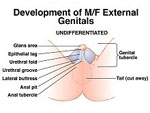
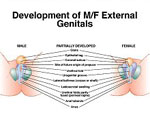
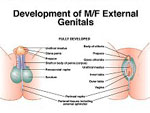
Doctors have a list of "standards" according to which they determine the "normality" of a newborn's genitalia, which includes two functional assessments of the adequacy of phallus size. One criteria is that the doctors believe young boys should be able to pee standing up and thus to 'feel normal' during little-boy peeing contests; adult men, meanwhile, need a penis big enough for vaginal penetration during sexual intercourse. The assignment of a genetically male baby as a girl is often due to a badly damaged or undeveloped penis - surgeons can make a vagina relatively easily but it is hard to make a penis that is functional. Underdeveloped penises are sometimes called a "Micropenis Condition" (also called Absent Penis, Buried Penis, Concealed Penis, Hidden Penis, Inconspicuous Penis, or Penile Agenesis, Trapped Penis, or Webbed Penis). Boys are typically born with a stretched penis ranging in length from 2.9 to 4.5 centimeters (1.25 to 1.75 inches), with a urethra opening at the tip (rather than on the side or base of the penis) that releases urine, and a scrotum that contains testes. For new-born girls, clitoral length at birth typically ranges from 0.2 to 0.85 centimeters (0.08 to 0.33 inches). Those falling in between these two sizes will often have their organs shortened. A clitoris longer than 1 centimeter is considered "unacceptably enlarged" and may be shaved down purely for purposes of looking "normal." On the other hand if the penis is less than 2.0 centimeters long, concern is often expressed about whether the boy will be a "boy".
A penis less than 1.5 centimeters long and 0.7 centimeters wide is usually considered to be "unacceptably short" and "inadequate for later sexual performance" and is usually deemed a clitoris, and he a "she." In this instance, although a genetically "XY" male, perhaps even with testes, the infant will be re-assigned as female and her "micropenis" surgically altered to become a clitoris. Such re-assignment is particularly likely if also the urethra does not open at the tip of the phallus, a common condition known as hypospadias. "If a baby has hypospadias, the urinary function will not be the same as other males," says Dr. Aydin Arici, a Yale-New Haven Hospital obstetrician and gynaecologist who specialises in reproductive endocrinology, explaining why male babies with such a condition might be reassigned. "For example, that individual will not be able to urinate standing up." Note that in most such cases urination is still POSSIBLE, and such surgery is not "mecially necessary." It is performed only to conform the child to social dictates of "normality." It should also be noted that, according to the chart of "normality" used by doctors, the teminology "enlarged clitoris" or "micropenis," in fact, refer to the SAME antatomical structure. In a child with otherwise ambiguous genitlia (where neither testes nor ovaries appear to be present), other lab testing may be done to try and determine whether or not it is a "penis" or "clitoris" based on chromosomal makeup. In a chromosomally intersexed child it may still be impossible to determine whether the structure, and the child, is "male" or "female." Clearly the most important factors in the sex assignment of intersexed children are achieving a "normal" appearance of the genitalia in the assigned sex, and sexual function. If a male's phallus is deemed unlikely to be able to "perform" adequately, then re-assignment as a female may become the preferred medical choice. But appearance and sexual function is not the only factor used in sex assignment - many laboratory tests are also done to determine the child's genetics and potential for fertility. This is sometimes criticized as a "Procreation Prejudice" due to the assumption that EVERYONE wants to have children, and in many cases of reassignment the mere prescence of sex organs is no indicator of future fertility. In the vast majority of cases of significant ambiguity, however, a female assignment is made - perhaps sometimes for the sake of medical expediency. Some in the medical community quip "It's easier to dig a hole than to build a pole." But once a sexual assignment is made, it's effectively irreversible, especially if surgery must be performed. So, in summary, among the kinds of surgeries that might be performed on intersexed people are:
|
||||||||